Introduction
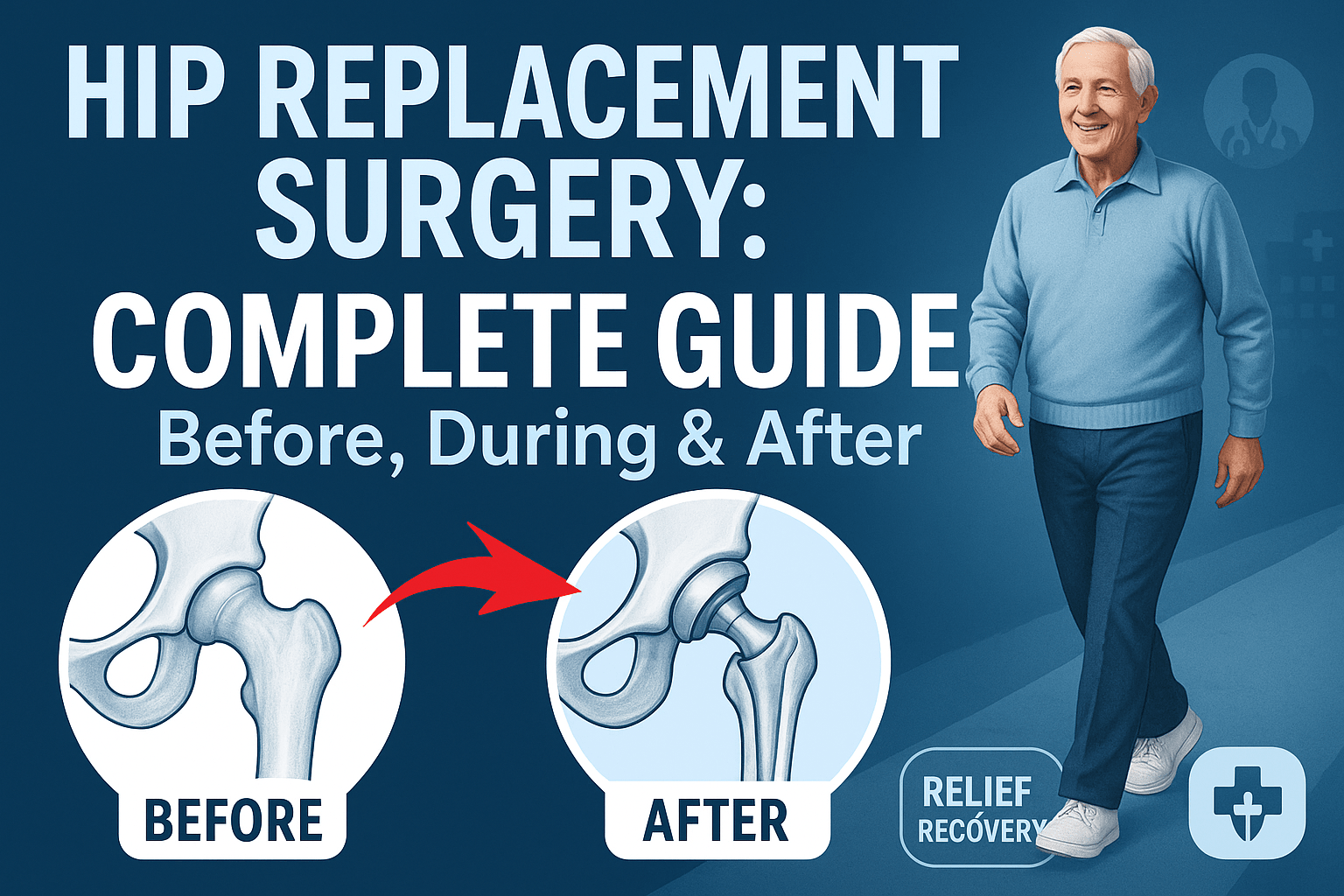
Hip replacement surgery (also called total hip arthroplasty) is a life-changing procedure for people suffering from chronic hip pain and stiffness due to arthritis, injury, or other degenerative conditions. Every year, hundreds of thousands of people undergo this surgery to regain mobility and improve their quality of life.
If you or a loved one is considering hip replacement, this comprehensive guide will walk you through everything you need to know—from pre-surgery preparation to post-operative recovery—so you can feel confident and well-informed every step of the way.
1. Understanding Hip Replacement Surgery
What Is Hip Replacement Surgery?
Hip replacement surgery involves removing a damaged hip joint and replacing it with an artificial implant made of durable materials like metal, ceramic, or medical-grade plastic. The goal is to:
- Eliminate chronic pain
- Restore joint function
- Improve mobility and flexibility
Who Needs a Hip Replacement?
Common reasons for hip replacement include:
✔ Osteoarthritis (wear-and-tear arthritis, most common cause)
✔ Rheumatoid arthritis (autoimmune joint damage)
✔ Osteonecrosis (bone death due to poor blood supply)
✔ Hip fractures (especially in elderly patients)
✔ Congenital hip disorders (developmental hip dysplasia)
If pain medications, physical therapy, or injections no longer provide relief, your doctor may recommend surgery.
2. Before Surgery: How to Prepare
Medical Evaluation & Tests
Before scheduling surgery, your doctor will perform:
- Physical examination (to assess overall health)
- Blood tests & imaging (X-rays, MRI, or CT scans)
- Cardiac evaluation (if you have heart conditions)
Lifestyle Adjustments for Better Recovery
- Quit smoking (smoking slows healing)
- Lose excess weight (reduces stress on the new joint)
- Strengthen muscles (physical therapy before surgery helps recovery)
Preparing Your Home for Post-Surgery Comfort
- Install safety aids (grab bars, shower seat, raised toilet seat)
- Remove trip hazards (loose rugs, clutter)
- Set up a recovery area (easy access to essentials)
What to Pack for the Hospital
- Loose, comfortable clothing (easy to put on)
- Slip-on shoes (no bending required)
- Personal toiletries (toothbrush, glasses, medications list)
3. During Surgery: What Happens in the Operating Room?
Types of Hip Replacement Surgeries
- Total Hip Replacement (THR) – Most common; replaces both the ball (femoral head) and socket (acetabulum).
- Partial Hip Replacement – Only replaces the femoral head (common after hip fractures).
- Minimally Invasive Hip Replacement – Smaller incisions, less muscle damage, faster recovery.
Step-by-Step Surgical Procedure
- Anesthesia – You’ll receive general anesthesia (fully asleep) or spinal anesthesia (awake but numb below the waist).
- Incision – The surgeon makes a 6-10 inch cut (smaller for minimally invasive).
- Damaged Bone Removal – The femoral head and damaged cartilage are removed.
- Implant Placement – A metal stem is inserted into the femur, and a prosthetic ball and socket are secured.
- Closure – The incision is stitched or stapled, and a sterile bandage is applied.
Surgery Duration: Typically 1-2 hours.
Anesthesia & Pain Management
- During surgery: Anesthesia ensures no pain.
- After surgery: You’ll receive IV painkillers, transitioning to oral medications as you recover.
4. After Surgery: Recovery & Rehabilitation
Hospital Stay (1-3 Days)
- Day 1: You’ll start walking with assistance (walker or crutches).
- Pain control: Medications and ice packs help manage discomfort.
- Blood clot prevention: Compression stockings and blood thinners are used.
First 2 Weeks at Home
- Mobility: Use a walker or cane as instructed.
- Wound care: Keep the incision clean and dry; watch for signs of infection.
- Activity restrictions: Avoid bending past 90°, crossing legs, or twisting.
Physical Therapy & Exercises
- Early exercises (first week): Ankle pumps, thigh squeezes.
- Weeks 2-6: Leg lifts, seated marches, gentle walking.
- After 6 weeks: Gradual return to normal activities.
Long-Term Recovery (3-12 Months)
- Full recovery time: 6-12 months (varies by individual).
- Driving: Usually allowed after 4-6 weeks.
- Returning to work: Desk jobs may resume earlier; physically demanding jobs may require 3+ months.
- Exercise & sports: Low-impact activities (swimming, cycling) are encouraged.
5. Risks & Possible Complications
While hip replacement is generally safe, potential risks include:
⚠ Infection (treated with antibiotics)
⚠ Blood clots (prevented with blood thinners)
⚠ Dislocation (avoid extreme movements early on)
⚠ Leg length discrepancy (rare, may require adjustments)
⚠ Implant loosening over time (may need revision surgery after 15+ years)
6. Tips for a Successful Recovery
✅ Follow all post-op instructions (medications, therapy, restrictions)
✅ Eat a protein-rich diet (helps tissue repair)
✅ Stay active but avoid high-impact activities (running, jumping)
✅ Attend all follow-up appointments (monitors healing progress)
7. Frequently Asked Questions (FAQs)
Q: How long does a hip replacement last?
A: Most last 15-20 years, but some can last longer with proper care.
Q: When can I sleep on my side after surgery?
A: Usually after 6 weeks, with a pillow between your legs.
Q: Can I kneel after hip replacement?
A: Yes, but wait until fully healed (3+ months) to avoid strain.
Q: Will I set off airport metal detectors?
A: Some implants may trigger them; carrying a medical ID card is helpful.
Conclusion
Hip replacement surgery can significantly improve your quality of life by relieving pain and restoring mobility. While recovery takes time and effort, following your doctor’s advice and staying committed to rehabilitation will help you return to an active, pain-free lifestyle.
If you’re considering hip replacement, consult an orthopedic specialist to discuss the best options for your needs.